Introduction
The anterior teeth tend to bear the brunt of many impact injuries. The position of maxillary incisors and their eruptive pattern carries a significant risk for trauma.[1] In many cases, the injury causes cessation of tooth development. Treatment of the immature nonvital anterior tooth presents several treatment challenges. The mechanical cleaning and shaping of a tooth with blunderbuss canal are difficult ; the thin fragile lateral dentinal walls can fracture during mechanical filing, and the large volume of necrotic debris contained in a wide root canal is difficult to completely disinfect.[2] Endodontic management of such teeth includes surgery and retrograde sealing, calcium hydroxide–induced apical closure (apexification) and more recently, placement of an apical plug of mineral trioxide aggregate (MTA) and gutta-percha obturation.[3] Most of the clinicians rely on traditional apexification .Mineral trioxide aggregate (MTA) has been used to provide an artificial barrier; however, it also has the limitations of non-reinforcement of root canal dentin and a high cost[4]. A novel concept of revascularization of immature nonvital, infected teeth was introduced to overcome the limitations. The authors have termed this regenerative process as revascularization, revitalization or maturogenesis. The common aspect of all regenerative modalities is intra canal disinfection using copious irrigation, placement of antibiotic pastes and formation of a sterile blood clot inside the pulp cavity[5]
Till date few cases have been reported using pulp regeneration as a therapeutic therapy for the treatment of immature non vital teeth.[4] It is difficult to clinically find bilateral non-vital, immature, infected teeth with approximately similar root development stage. A case report is presented with bilateral immature central incisors treated with apical barrier formation with MTA and pulp revascularization induced maturation procedures.
Case Report
A 9 year old male child reported to the out patient department of Pediatric and Preventive Dentistry in Guru Nanak Dev Dental College & Research Institute, Sunam with severe pain in upper front teeth region. Child had suffered a traumatic injury to the maxillary central incisors about one month ago with loss of coronal fragments. He went to the local dentist & was given symptomatic treatment for the same . His medical history was non contributory .Radiographic examination revealed pulp exposures in both the incisors with immature apices (Figure 1). Restoration was seen in right maxillary central incisor .A diagnosis of immature non-vital maxillary central incisors was made. It was planned to perform apexification with MTA followed by gutta-percha obturation in left maxillary central incisor and revascularization procedure in right maxillary central incisor. Patient was explained all risks and benefits of procedures and an informed written consent was obtained.
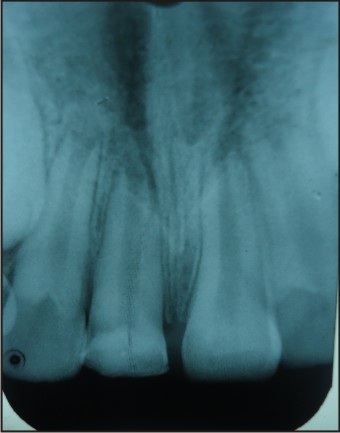 | Fig 1 : Pre-operative radiograph showing teeth (21,11) with open apex.
 |
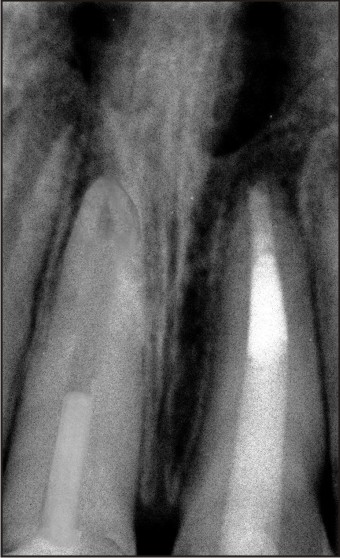
In the first appointment , After proper isolation with rubber dam ,Access opening was done in both the incisors & minimal instrumentation was done with k-type files. Irrigation was done with 5% NaOCl and 3% hydrogen peroxide. A sterile cotton pellet was placed in the pulp chamber & access cavity was sealed with a temporary restorative material. After 3 days patient was recalled & root canal system was reentered. Working length was estimated with the help of intra-oral peri-apical radiographs. In left maxillary central incisor , MTA (Dentsply) was placed in apical region and a 4mm barrier was made (Figure 2) In maxillary right central incisor triple antibiotic paste with antimicrobial agents of equal parts of metronidazole, minocycline and ciprofloxacin was placed carefully with the help of hand plugger. The access cavity was sealed. The patient was recalled after 3 weeks for next appointment of revascularization procedure in right maxillary incisor. In the following appointment, the revascularization process was completed as follows; after rubber dam application , the intracanal medicament was flushed with saline and 5.25% sodium hypochlorite solution. The canal system was dried with absorbent paper points. A sterile 23-gauge needle was taken and a rubber stopper was placed at 2 mm beyond the working length. With sharp strokes, the needle was pushed past the confines of the canal into the periapical tissue to intentionally induce bleeding into the canal. When frank bleeding was evident at the cervical portion of the root canal system, a tight dry cotton pellet was inserted at a depth of 3– 4 mm into the canal and the pulp chamber and held there for 7–10 minutes to allow formation of clot in the root canal. The access opening was sealed with MTA extending 4 mm into the coronal portion of the root canal system. An intraoral radiograph was taken for a baseline record (Figure 3) . Mean while, conventional gutta percha obturation was done followed by Fibre post (3M) placement in left maxillary central incisor . Both the central incisors were kept on regular follow up. After 6 months, lateral dentinal thickening was first noticed in 11, whereas no such thickening was noticed in 21 (Figure 4). Both the teeth were kept on regular follow up for 6, 9,12, 15 & 18 months. (Figure 5 & 6) At the end of 18 months, Complete root formation was seen in 11 with lateral dentinal wall thickening .No such thickening was seen in 21 but both the teeth were healthy and symptom free.
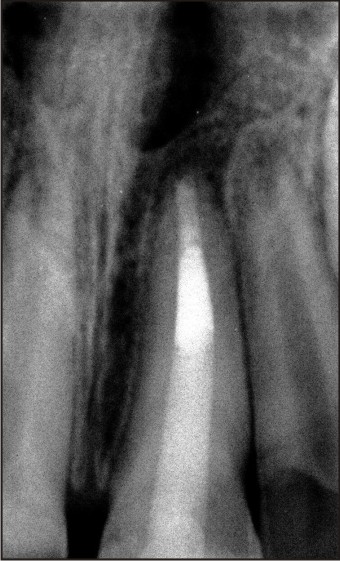 | Fig 2 : Radiovisiograph after MTA plug & post placement in 21.
 |
 | Fig 3 : Base line radiovisiograph showing revascularization wrt 11 .
 |
 | Fig 4 : Radiovisiograph taken after 6 months. Signs of apical closure and dentin bridge formation were observed in 11 .
 |
 | Fig 5 : Radiovisiograph after 12 months .
 |
 | Fig 6 : Post-operative radiovisiograph at 18 months .Completion of root apex and lateral dentinal wall thickening were seen in 11 & no such changes were seen in 21.
 |
Discussion
Recent advances in the field of regenerative medicine have inspired the dental researchers to look beyond just replacement of damaged tissues, and the researchers are now trying to develop methods to regenerate them, rather than just replacing.[4] A major challenge faced by most the dentists is the treatment of thin, fragile blunderbuss canals in non vital teeth.[2] Traditionally, the only regenerative therapy available in such cases was apexification using long term calcium hydroxide therapy. Various clinical studies had demonstrated the efficacy of Ca(OH)2 in apexification.[6] However, all the case reports and studies have documented only apical closure. There was no root elongation or maturation and all cases required subsequent root canal obturation. Ca(OH) 2 therapy was also shown to pose a threat of root fracture in 77% of immature teeth. Also because of its high pH, it could damage the cells with regenerative capacity. [7] Various other materials have been tried to induce apexification, such as tricalcium phosphate, collagen calcium phosphate, osteogenic protein-1 and mineral trioxide aggregate.[8] However, none of the above mentioned methods lead to root elongation or maturation. Apical plug of mineral trioxide aggregate (MTA) and guttapercha filling is currently the clinician's choice and it has several advantages over calcium hydroxide induced apexification.[9], [10], [11], [12] MTA is a biocompatible material, has osteo-inductive properties, sets in the presence of moisture and the treatment can be completed in a single sitting. However, it does not strengthen the remaining tooth structure. The novel procedure of revascularization exploits the full potential of the pulp for dentine deposition and produces a stronger mature root that is better able to withstand fracture[13]
The revascularization of non vital teeth has been demonstrated earlier in replanted teeth with open apices. Using the same concept, revitalization of a non vital immature tooth was attempted in the present study by creating a sterile blood clot in the pulp space. The blood clot acted as a matrix onto which the vital cells from peri-apex could get seeded and reestablish the pulp vascularity.[4] The most plausible mechanism of the root development is the isolation of stem cells from SCAP. It has been hypothesized that SCAP can be the source of primary odontoblasts forming the root dentin.[2],[9]
The present case simultaneously evaluated MTA apexification and obturation, with revascularization induced maturogenesis. Response to pulp vitality tests, clinical examinations and purulent discharge on access opening indicated pulpal necrosis and infection.
A critical step in regenerative therapy is complete disinfection of the root canal space using copious irrigation, minimal instrumentation and placement of antibiotic pastes.[14],[15]
This regenerative therapy can provide advantage over traditional apexification as there is elongation as well as strengthening of the root due to reinforcement of lateral dentinal walls, with deposition of new dentin/hard tissue. There are certain limitations to this approach such as: Bleeding into the canal space is necessary, and this treatment option is not indicated in cases where post and core is the final restorative treatment plan, as the vital tissue in apical 2/3 rd of the canal cannot be violated for post placement [2],[16]
In conclusion, revascularization induced maturogenesis, where indicated, can provide several advantages over conventional apexification procedures. A detailed histo-pathological study is necessary to demonstrate the actual contents of pulp space after revascularization procedures.
Conclusion
Although MTA has excellent sealing ability and is a promising material for apical barrier formation ,it does not allow lateral dentinal wall thickening. Revascularization helps in development and reinforcement of dentinal walls by deposition of hard tissue, thus strengthening the root against fracture. It is also very cost-effective, because no additional material (such as TCP, MTA) is required . Still further studies should be carried out to prove the efficacy of this procedure over MTA apexification.
References
1. P Goenka, N Marwah, S Dutta.Biological approach for management of anterior tooth trauma: Triple case report.J Indian Soc Pedod Prev Dent. 2010;28(3):223-29
2. Shah N ,Logani A, Bhaskar U, Aggarwal V. Efficacy of Revascularization to Induce Apexification / Apexogensis in Infected, Nonvital, Immature Teeth: A Pilot Clinical Study. J Endod. 2008;34:919–925
3. Archana S.M, Sujana V, Nagesh B, Krishna Babu P.J .Revascularisation- an overview . J Int Dent Med Res 2012;5(1):55-59.
4. Aggarwal V., Miglani S & Singla M. Conventional apexification and revascularization induced maturogenesis of two non-vital, immature teeth in same patient: 24 months follow up of a case. J Conserv Dent.2012;15(1):68-72.
5. George T-J Huang. A paradigm shift in endodontic management of immature teeth: conservation of stem cells for regeneration. J Dent. 2008; 36(6):379-86.
6. Kleier DJ, Barr ES. A study of endodontically apexified teeth. Endod Dent Traumatol. 1991;7:112.
7. Andreasen JO, Farik B, Munksgaard. Long-term calcium hydroxide as a root canal dressing may increase the risk of root fracture. Dent Trautamol. 2002;18:134–7
8. Shabahang S, Torabinejad M, Boyne PP, Abedi H, McMillan P. A comparative study ofroot-end induction using osteogenic protein-I, calcium hydroxide and mineral trioxideaggregate in dogs. J Endod. 1999;25:1–5.
9. Farsi N, Abuzeid S, Ashiry E. Revascularization of Dental Pulp In Human Necrotic Permanent Teeth with Immature Apex: three case reports. Life Science Journal 2013;10(3)
10. Torabinejad M, Parirokh M. Mineral trioxide aggregate: a comprehensive literature review—Part II: Leakage and biocompatibility investigations. J Endod 2010; 36(2):190–202. 15.
11. Elisabetta Cotti, Manuela Mereu, Daniela Lusso. Regenerative treatment of an immature, traumatized tooth with apical periodontitis: Report of a case. J Endod 2008; 34: 611-616. 16.
12. Fuks A. B., “Vital pulp therapy with new materials for primary teeth: new directions and treatment perspectives. Pediatric Dentistry 2008; 30(3):211–219.
13. Reynolds K, Johnson JD, Cohenca N: Pulp revascularization of necrotic bilateral bicuspids using a modified novel technique to eliminate potential coronal discolouration: a case report. International Endodontic Journal, 2009, 42, 84–92.
14. Iwaya S, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol. 2001;17:185-7.
15. Windley W, Teixeira F, Levin L, Sigurdsson A, Trope M: Disinfection of Immature Teeth with a Triple Antibiotic Paste. JOE June 2005, 31 (6): 439- 443.
16. Ding RY, Cheung GS, Chen J, Yin XZ, Wang QQ, Zhang CF. Pulp revascularization of immature teeth with apical periodontitis : A clinical study. J Endod. 2009;35:745–9.
|